Oncogenic virus: Scientists show how HPV causes skin cancer
Viruses are thought to play a role in the development of about 10 percent of human cancers. An international research team led by scientists in Vienna now showed that human papillomavirus 42 (HPV42) drives the development of a certain type of skin cancer. The findings, reported in the journal Cancer Discovery, will be important for future research into prevention, diagnosis, and therapy.
Viruses have taken centre stage in science-related news in the past few years. The infectious diseases that they can cause - from COVID-19 to AIDS and Ebola - are notorious. In the public eye, however, much less attention is given to the fact that viruses can also cause cancer. Scientists think that viruses play a role in about 10 percent of all human cancers. However, if and how viruses contribute to skin cancers has not been systematically studied.
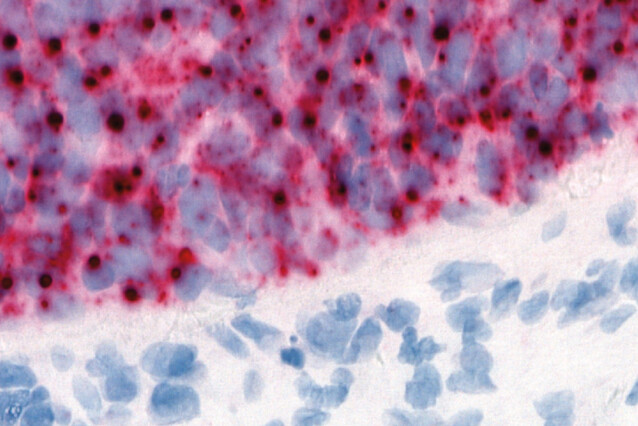
An international research team led by Anna Obenauf of the Research Institute of Molecular Pathology and Thomas Wiesner of the Medical University of Vienna set out to address this knowledge gap. The team decided to focus on skin cancers with unknown causes, as human skin is constantly exposed to viruses. There are more than 6,000 viruses that can infect vertebrates. Using publicly available data of cancer genomes, the scientists could screen for the presence of each of these 6,000 viruses in 19 different types of skin cancer. In 96 percent of the analysed samples of Digital Papillary Adenocarcinoma or DPA, an aggressive type of skin cancer that occurs mainly on fingers and toes, they found human papilloma virus 42 (HPV42).
Human papillomavirus is a common DNA virus with over 220 known types. Their involvement in causing various kinds of cancer is long established: as early as 1976, Harald zur Hausen studied links between certain HPV types and cervical cancer, which led to him receiving a Nobel Prize in 2008. Common vaccination schemes protect very well against sexually transmitted HPVs and their cancer-causing effects. It is possible, however, that other cancer-causing HPVs have been neglected. HPV42, for instance, has been considered harmless so far.
The scientists now turned to unravelling the detailed cellular mechanisms triggered by HPV42. Using a combination of functional experiments, the scientists found that HPV42 indeed had cancer-causing effects in model systems. They developed an innovative machine learning algorithm that allowed them to screen for genes whose expression is altered by HPV42 and other cancer-causing HPV types. In samples infected by HPV42, they found that a viral oncogene called E7 activates a set of genes in a way that is specific to HPV-driven cancers, which does not occur in benign warts also caused by HPV infections. The researchers showed that this change in gene expression involves at least 12 genes and is induced by all known oncogenic HPVs. Intriguingly, it resembles a transcriptional program of germ cells in testes.
“The network of genes that we identified makes the difference between cancers caused by HPVs and others,” says Thomas Wiesner. “Although DPA is relatively rare, our findings give valuable insights into how HPV viruses can cause tumours to grow.”
Understanding the molecular basis of a patient’s cancer can be crucial for diagnosis and therapy. For instance, neck and head cancers can be caused by HPV, but they can also originate from mutations – this distinction determines how aggressive the treatment needs to be. Current diagnostic tools for these cancers wrongly classify about 10 percent of patients as HPV-positive when they are actually not. To address this issue, the scientists sifted through the HPV-specific gene network to identify genes that can be used to distinguish HPV-driven cancers from the others. With only two genes, they were able to improve accurate classification from 85 to 97 percent of HPV-driven cancers – a major improvement for diagnosis.
In addition to preventing and diagnosing cancers, the findings point out a potential target for treating HPV-caused cancers via immunotherapy. “Some of the genes involved in this HPV-induced program have properties that make them possible targets for the immune system,” says Anna Obenauf. “These genes are only expressed in HPV-positive cancers and in germ cells, but not in other healthy somatic tissues. They could be promising target molecules for therapeutic cancer vaccines or immunotherapies.”
Original Publication
Lukas Leiendecker, Tobias Neumann, Pauline S. Jung, Shona M. Cronin, Thomas L. Steinacker, Alexander Schleiffer, Michael Schutzbier, Karl Mechtler, Thibault Kervarrec, Estelle Laurent, Kamel Bachiri, Etienne Coyaud, Rajmohan Murali, Klaus J. Busam, Babak Itzinger-Monshi, Reinhard Kirnbauer, Lorenzo Cerroni, Eduardo Calonje, Arno Rütten, Frank Stubenrauch, Klaus G. Griewank, Thomas Wiesner, Anna C. Obenauf:
“Human papillomavirus 42 drives digital papillary adenocarcinoma and elicits a germ-cell like program conserved in HPV-positive cancers”. Cancer Discovery, 2022. DOI: https://doi.org/10.1158/2159-8290.CD-22-0489
About the IMP and Vienna BioCenter
The Research Institute of Molecular Pathology (IMP) in Vienna is a basic life science research institute largely sponsored by Boehringer Ingelheim. With over 200 scientists from 40 countries, the IMP is committed to scientific discovery of fundamental molecular and cellular mechanisms underlying complex biological phenomena. The IMP is part of the Vienna BioCenter, one of Europe’s most dynamic life science hubs with 2,650 people from over 80 countries in six research institutions, three universities, and 41 biotech companies. www.imp.ac.at, www.viennabiocenter.org
About the Medical University of Vienna
Medical University of Vienna (MedUni Vienna) is one of the most traditional medical education and research facilities in Europe. With almost 8,000 students, it is currently the largest medical training centre in the German-speaking countries. With 6,000 employees, 30 departments and two clinical institutes, 13 medical theory centres and numerous highly specialised laboratories, it is one of Europe's leading research establishments in the biomedical sector. MedUni Vienna also has a medical history museum, the Josephinum. https://www.meduniwien.ac.at/web/en/